#MedicalPhysicistOnTourPart1
One of the great things about the STP is the ability to parachute into other departments to have a look at how your decisions as a clinical scientist would affect the department’s working life. It also enables you to have a further insight into the workings of other parts of the hospital and how everyone fits together in the big picture beyond just doctors and nurses! Today I got the opportunity to spend the day in Echocardiography hanging out with cardiac physiologists performing ultrasounds of peoples’ hearts.
One of the best things about the day was discussing how the use of Artificial Intelligence will impact the role of echocardiographers.
Currently as part of the routine patient work-up, the volume of the Left Ventricle is measured and the ejection fraction is calculated. This involves manual drawing of a region of interest on the ultrasound images. Using 2D images, the variability between operators in ejection fraction calculated is approximately 10%. Using 3D images, this drops to 5%. This is a large decrease in variability and is important because when patients are undergoing chemotherapy, changes in ejection fraction of 10% would indicate poor response and chemo would be discontinued. This 10% could simply be operator dependent variation on 2D images. Using 3D images is preferred for this reason and the inherent uncertainty of estimating a 3D volume from 2D slices that can lead to over or under estimations of ejection fraction.
One of the limitations of using AI in ultrasound is the large operator dependency on the image quality along with the patient specific factors influencing image quality such as body habitus and lung fibrosis status. This variability inevitably makes training an algorithm more difficult than training an algorithm which is looking for say fluid on the lungs amongst thousands of chest x-rays all taken with the same kV and mA.
Artifical Intelligence is currently used to guess where the 2D boundaries of the heart lie with operators then tweaking the regions of interest to reflect the anatomy as they see fit. If this can be extended to 3D in a new software roll out then operators would have the best of both worlds! Decreased uncertainty from using 3D images vs 2D and decreased variability between operators if the AI can be relied upon to create the boundaries. This would then enable more effective tracking of ejection fraction during chemotherapy.
But enough about AI. (I kid, there will never be too much chat about AI!)
Here is a quick list of today’s take home messages gleaned from a day spent observing. These are relevant to both ultrasound and wider clinical practice:
- Aliasing of signal in ultrasound indicates turbulent blood flow.
- CPAP stands for Continuous Positive Airway Pressure. CPAP machines are used in those with obstructive sleep apnea and maintain a mid air pressure on a continuous basis to keep the airways open.
- When you turn up for a stress examination into the degree of blockage of your heart vessels having had the same test the year before, perhaps don’t voice thoughts such as “I should do some exercise, I thought this last year when I was puffing away on the treadmill” and “I don’t have time to go to the gym”……
- Chronic Obstructive Pulmonary Disease (COPD) patients have poorer image quality echocardiograms due to fluid on the lungs and fibrosis of the lungs.
- Mechanical atrial valve replacements tick audibly like clocks! They tend to last for 25 years+ or a patient’s lifetime whereas tissue valves last for 10-20 years. Patients with mechanical valves are at an increased risk of clotting and so are on anticoagulants for life.
- If you have a stress test booked that will involve exercise, maybe consider wearing a sports bra and something other than jeans.
- During stress testing, family members are not allowed into the room due to the risk of patient collapse.
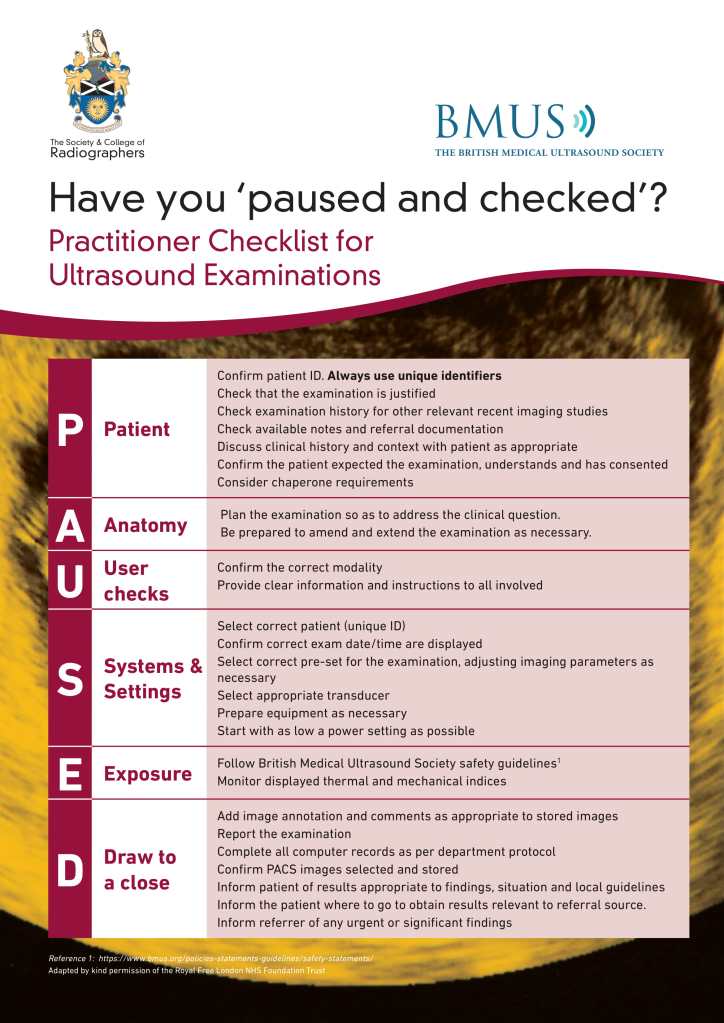
- Why are patients booked in for appointments in which the outcome will have literally no effect on their treatment plan or give any information in addition to what has been obtained recently?! Pause and Check should apply to all imaging modalities and diagnostic tests!
Pause and Check
Turns out there are some BMUS guidelines on Pause and Check but these are ultrasound practitioner specific and not referrer specific!
Tune in tomorrow for #MedicalPhysicistOnTourPart2!